41 medicare appeals process diagram
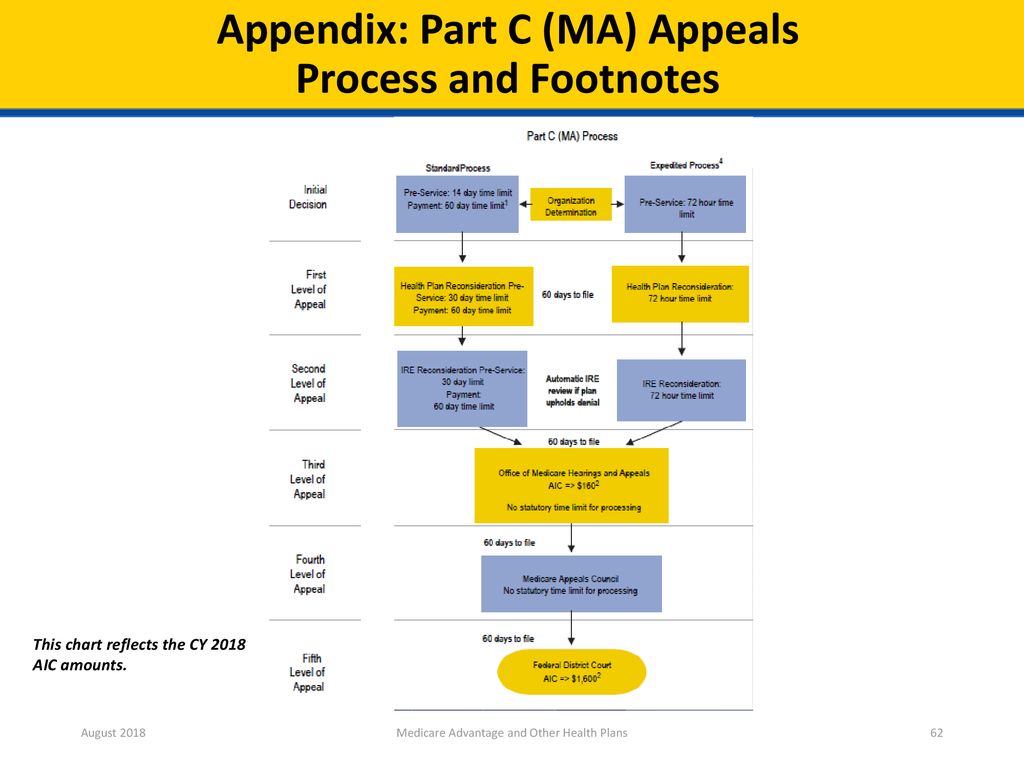
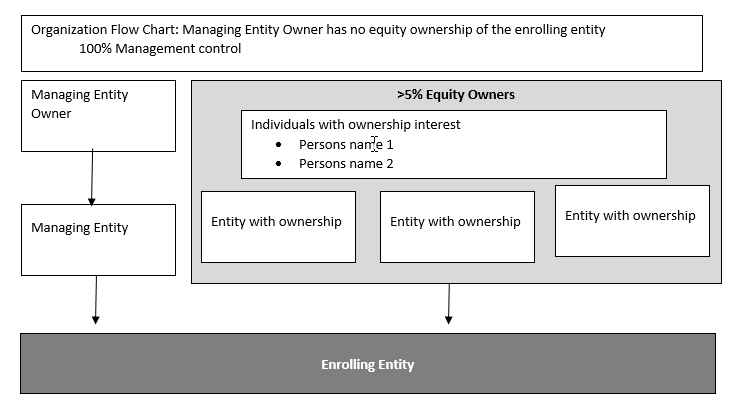
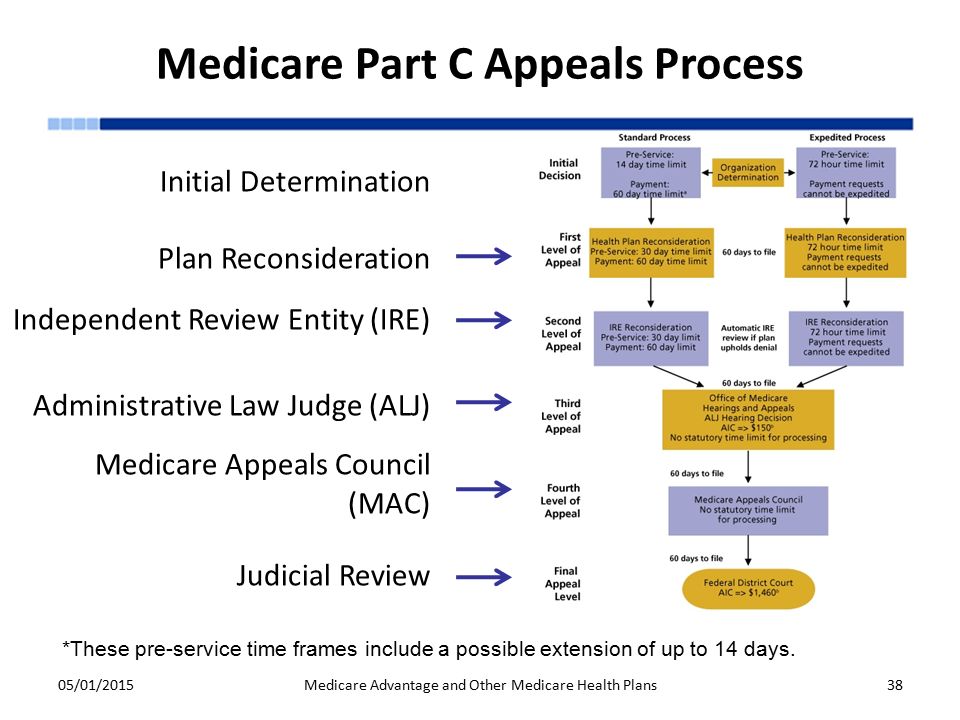
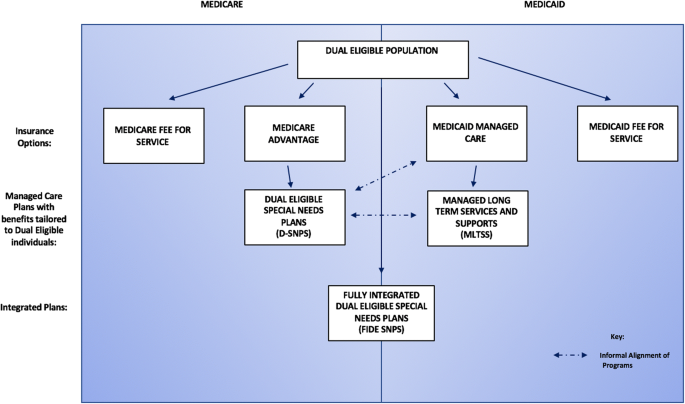
Process Map Symbols. Each step in a process is represented by a shape in a process map. These shapes are also called flowchart shapes. There are nearly 30 standard shapes that you can use in process mapping.However, we think for most people, using a handful of the most common shapes will be easier to understand. Medicare health plans, which include Medicare Advantage (MA) plans – such as Health Maintenance Organizations, Preferred Provider Organizations, Medical Savings Account plans and Private Fee-For-Service plans – Cost Plans and Health Care Prepayment Plans, must meet the requirements for grievance and appeals processing under Subpart M of the Medicare Advantage regulations.
22. Q: Does the Prior Authorization process require new coverage or documentation requirements? A: No. Prior authorization does not create new coverage or documentation requirements. Instead, regularly required documentation must be submitted earlier in the process. Separate from the prior authorization process, MACs may develop Local Coverage

Medicare appeals process diagram
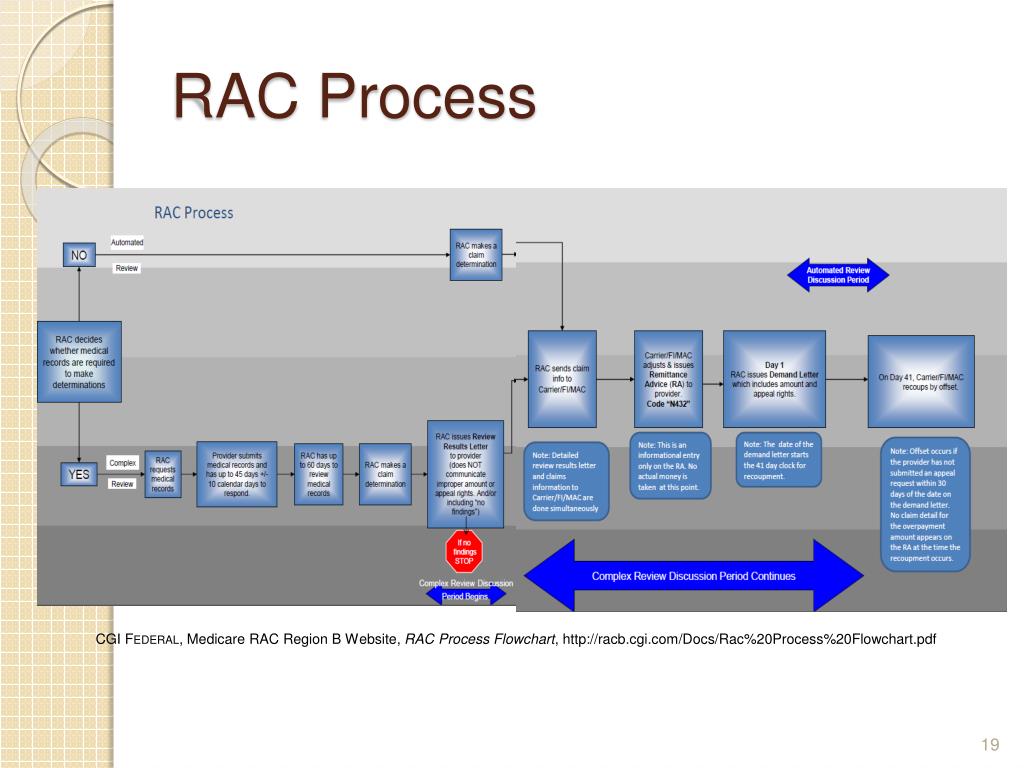
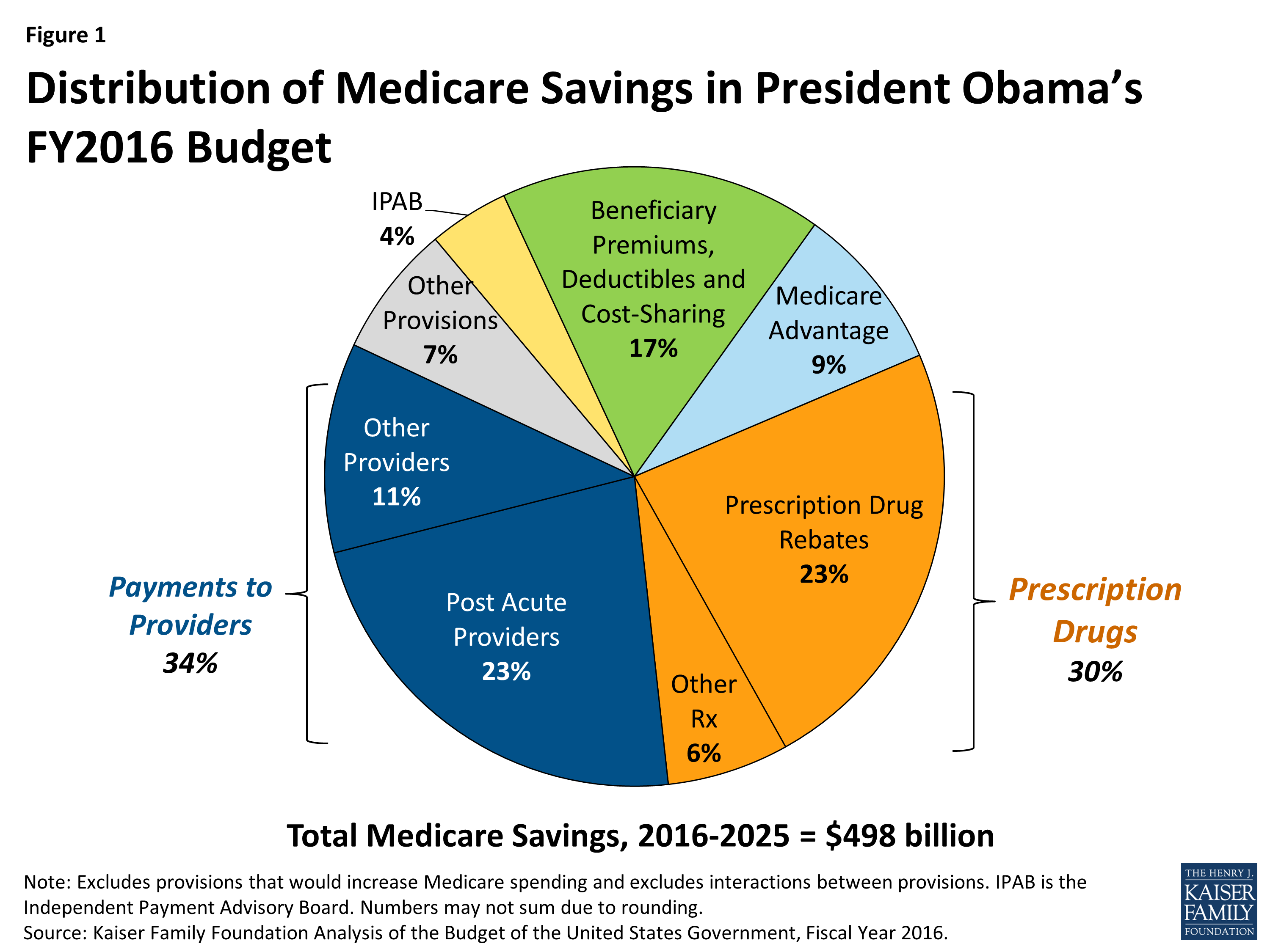
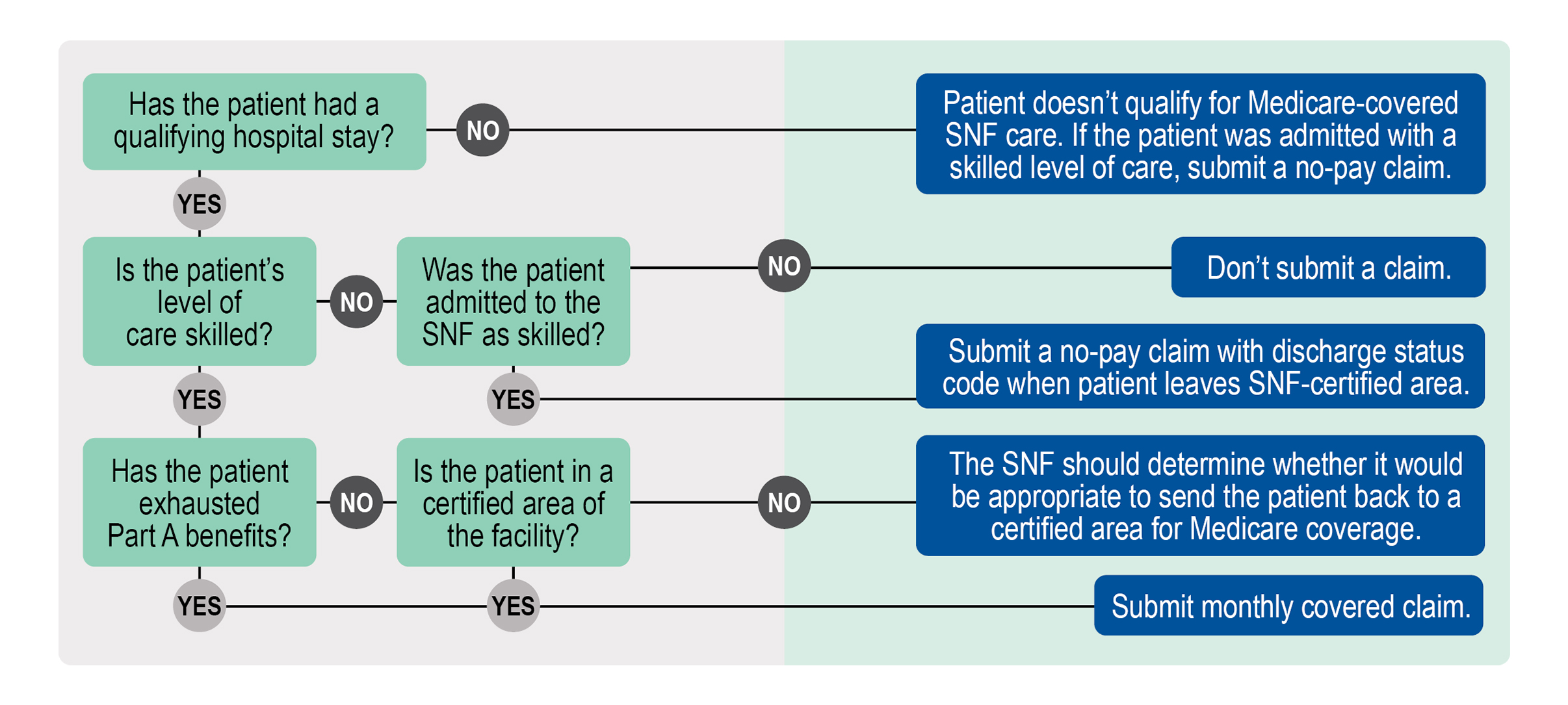
Claim denials from Medicare, Medicaid and health plans are on the rise, and understanding recent trends in denials is essential to the development of an effective and comprehensive appeal strategy. Among those emerging trends, distinguishing coding denials from clinical validation denials (CVDs) is an ongoing challenge. Medicare may offer you better payment rates, and coordinated health coverage may expedite the payment process and reduce administrative costs. Avoiding Medicare recovery efforts: Filing claims correctly the first time prevents future claim recovery efforts. To see a diagram (flowchart) of the original Medicare (fee-for-service) standard and expedited appeals process, go to the "Downloads" section below. Appointment of Representative A party may appoint any individual, including an attorney, to act as his or her representative during the processing of a claim(s) and /or any claim appeals.
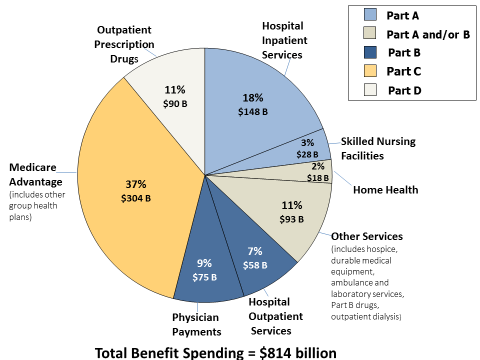
Medicare appeals process diagram. Generally, the different parts of Medicare help cover specific services. Most beneficiaries choose to receive their Part A and B benefits through Original Medicare, the traditional fee-for-service program offered directly through the federal government. It is sometimes called Traditional Medicare or Fee-for-Service (FFS) Medicare. Under Original Medicare, the government pays directly for the ... Organization Determinations, is any decision made by a Medicare health plan regarding receipt of, or payment for, a managed care item or service; the amount a health plan requires an enrollee to pay for an item or service; or a limit on the quantity of items or services. If you have a Medicare health plan, start the appeal process through your plan. Follow the directions in the plan's initial denial notice and plan materials. You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination. A review of denial and audit data can help providers prevent errors that lead to denials, and in the process reduce financial loss and increase resource efficiency. 3 emerging trends call for a proactive denial and appeal strategy. A proactive approach is essential to identifying root causes as the basis for denial management and prevention.
To see a diagram (flowchart) of the original Medicare (fee-for-service) standard and expedited appeals process, go to the "Downloads" section below. Appointment of Representative A party may appoint any individual, including an attorney, to act as his or her representative during the processing of a claim(s) and /or any claim appeals. Medicare may offer you better payment rates, and coordinated health coverage may expedite the payment process and reduce administrative costs. Avoiding Medicare recovery efforts: Filing claims correctly the first time prevents future claim recovery efforts. Claim denials from Medicare, Medicaid and health plans are on the rise, and understanding recent trends in denials is essential to the development of an effective and comprehensive appeal strategy. Among those emerging trends, distinguishing coding denials from clinical validation denials (CVDs) is an ongoing challenge.











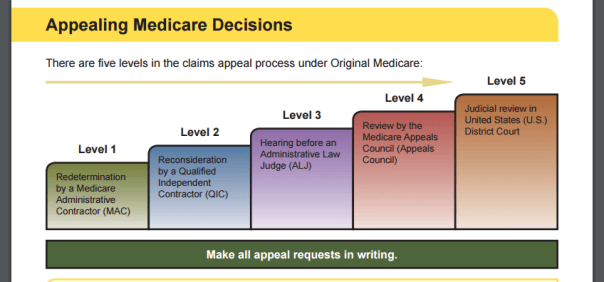




0 Response to "41 medicare appeals process diagram"
Post a Comment